The request from baby welfare authorities appeared innocent sufficient: Order a new child drug check. Dr. Sharon Ostfeld-Johns and her hospital colleagues had completed it numerous instances earlier than.
This time, nonetheless, the request gave the physician pause. A affected person at Yale New Haven Well being in Connecticut, the biggest well being system within the state, had stated that she’d used marijuana to assist her eat and sleep throughout her being pregnant. The hospital had reported her to baby welfare authorities. Now, an investigator needed Ostfeld-Johns to drug check the new child.
Ostfeld-Johns knew there was no medical purpose to check the newborn, who was wholesome. A drug check would make no distinction to the toddler’s medical care. Nor did she have considerations that the mom, who had different youngsters at residence, was a neglectful mother or father. The physician did fear, nonetheless, that the drug check may trigger different issues for the household. For instance, the mom was Black and on Medicaid — race and revenue bias may affect the investigator’s determination on whether or not to place the kids into foster care.
“Why did I ever order these checks?” Ostfeld-Johns discovered herself questioning, about previous circumstances. She considered her personal son, then in kindergarten, and the way she would really feel if she confronted an investigation over a constructive check. Ultimately, she would assessment her personal prenatal data and study that she had been examined for medicine with out her data or consent. “You attempt to think about what it will be like if it was you,” she stated. “The harm that we do to individuals is overwhelming.”
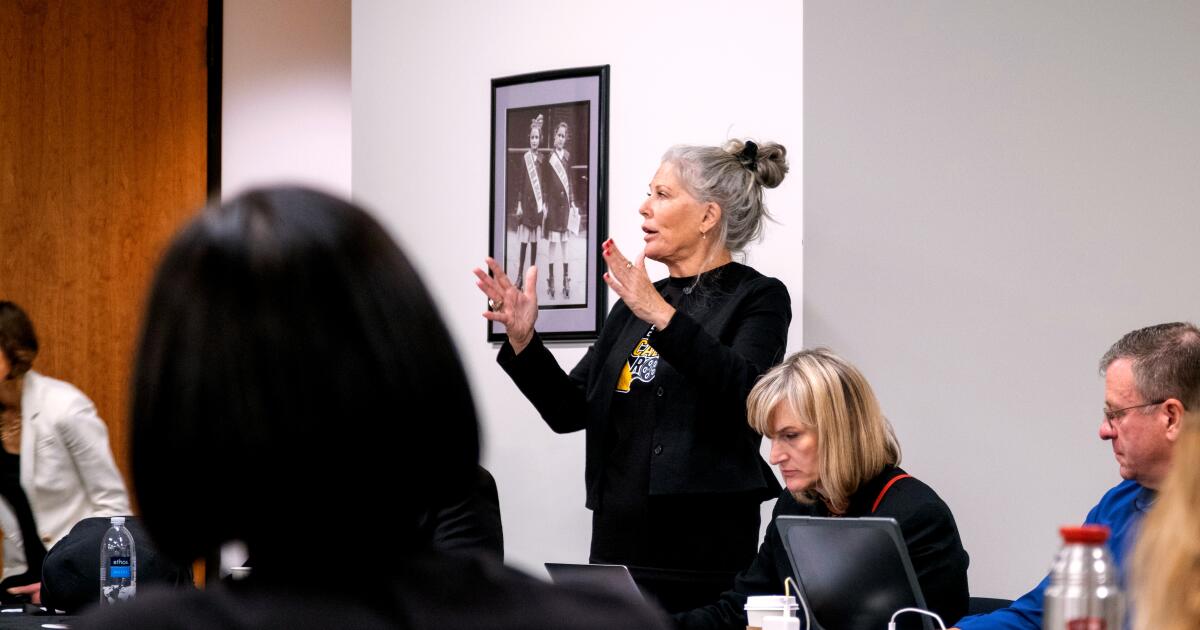
Ostfeld-Johns had encountered this state of affairs many instances earlier than, however this time, she refused the drug check request. Then she started a analysis course of that, in 2022, led to an overhaul of the Yale New Haven Well being community’s strategy to drug testing newborns. Now, docs are directed to check provided that doing so will inform medical care — a uncommon incidence, it seems. The hospital additionally created standards for testing pregnant sufferers.
Many docs and nurses throughout the nation have lengthy assumed that drug testing is each a medical and authorized necessity of their care of pregnant sufferers and newborns — regardless that most state legal guidelines don’t require it. But drug testing throughout labor is widespread in America, with a constructive check usually triggering a report back to baby welfare authorities. Ostfeld-Johns and Yale New Haven are amongst a small however growing variety of docs and establishments throughout the nation which have began questioning these drug-testing insurance policies. This cadre of docs is pushing hospitals to grow to be much less reliant on checks and to focus as an alternative on speaking immediately with sufferers to evaluate any dangers to infants.
Nobody appears to be monitoring simply what number of hospitals have revised their testing insurance policies, however over the previous three years, modifications have come to networks throughout the nation, from California to Colorado to Massachusetts. The establishments differ, from massive nonprofit networks and educating services to non-public, for-profit hospitals.
Whereas docs pushing for reform argue that laws remains to be wanted to require hospitals to cut back testing, particular person hospital efforts appear to be spreading. In Colorado, docs labored with a baby abuse prevention nonprofit to distribute a voluntary new coverage as steering, prompting a number of hospitals to vary their practices. An academic effort, “Doing Proper by Beginning,” convened digital teams of well being care professionals throughout the nation in 2023, to show them their necessities below the regulation. Some members have been stunned to study that almost all state legal guidelines don’t really require hospitals to drug check pregnant sufferers or newborns, and at the moment are questioning the insurance policies of their establishments, suggesting extra reforms could come.
At Yale, Ostfeld-Johns stated she initially confronted resistance to the coverage change. A few of her colleagues feared that by ending near-automatic testing, “we have been in the end going to harm infants,” she stated. “We have been hurting them by stopping identification of substance publicity that occurred throughout being pregnant.” However Ostfeld-Johns stated they discovered they didn’t want the drug checks to establish infants who would possibly, for instance, develop signs of opioid withdrawal that might require particular care.
On the New Haven hospital, the coverage change seems to have curbed pointless baby welfare studies with out harming infants. After the coverage went into impact, baby welfare referrals from the new child nursery dropped nearly 50%, in accordance with preliminary knowledge offered by Ostfeld-Johns. On the similar time, the hospital didn’t see an uptick in infants coming again in want of recent remedy for drug withdrawal, she stated. “No infants got here in with uncontrolled withdrawal signs,” she stated. “No security occasions have been recognized.”
The New Haven knowledge is in line with the anecdotal experiences of suppliers at different establishments. “I don’t assume we’re lacking infants” who’ve been uncovered to substances, stated Dr. Mark Vining, the director of the new child nursery at UMass Memorial Medical Middle close to Boston. The hospital did away with automated testing of newborns in 2024. On the similar time, Vining stated, it has reported fewer households to baby welfare authorities on account of constructive checks brought on by hospital-administered medicines, like morphine. A new child drug check “hardly ever provides any info that you simply didn’t already know,” he stated.
The brand new insurance policies are starting to upend an strategy that has existed in the USA for many years.
Hospitals first started routinely drug testing moms in labor in the course of the Nineteen Eighties crack cocaine epidemic. The follow expanded in the course of the opioid epidemic, following the passage of a federal regulation in 2003 and one other in 2016, each of which require hospitals to inform baby welfare companies anytime a child is born “affected by” substances. Federal regulation and legal guidelines in most states don’t require hospitals to drug check new mother and father or their infants, however hospitals incessantly accomplish that anyway — usually out of concern that in the event that they don’t, they’ll miss infants who’re in danger.
Widespread drug testing has induced quite a lot of harms. A earlier investigation by The Marshall Challenge discovered that urine checks, the sort utilized by most hospitals, are straightforward to misread and have false constructive charges as excessive as 50%. Mother and father have been reported to baby welfare authorities over false positives brought on by issues starting from poppy seeds to blood strain remedy. Substances prescribed to sufferers throughout a hospital keep, such because the fentanyl in an epidural, can present up on maternal drug checks and in addition move shortly from mom to child, inflicting infants to check constructive for medicine.

Poppy seeds, utilized in bagels, salads and different meals, can yield constructive outcomes for opiates in urine checks.
Race and sophistication bias may also affect drug testing, with a number of research discovering that low-income, Black, Latina and indigenous girls are most definitely to be examined. Yale New Haven Hospital discovered that, earlier than the drug testing coverage change, Black infants in its care have been twice as possible as White infants to be examined at start. Research elsewhere have discovered that racial disparities prolong to baby welfare circumstances and removals as effectively, with Black, Latino and indigenous infants being much less prone to be reunited with their mother and father as soon as eliminated.
In lots of hospitals, the checks should not usually used to make medical selections. As a substitute, checks have grow to be an affordable, quick solution to assess whether or not a mother or father is perhaps a hazard to their baby.
“We must be doing medical checks for medical causes, not felony, punitive, prosecutorial causes,” stated Dr. Christine Gold, a pediatrician who works on the College of Colorado Hospital system close to Denver. Even for that function, Gold famous, drug checks fall brief. “It’s a actually poor-quality check,” she stated. It can’t inform docs how usually somebody used a substance throughout being pregnant, if a affected person has an habit or if the drug use impacted their capability to mother or father. “Toxicology checks should not parenting checks,” Gold stated.
In 2020, Colorado lawmakers eliminated constructive drug checks at start from the listing of causes for hospitals to routinely report a household to baby welfare authorities. However many hospitals continued to check pregnant sufferers and newborns, prompting Gold to steer the hassle to launch steering in 2023 that encourages hospitals within the state to check solely when medically crucial. Now the whole College of Colorado Well being system is reforming its coverage on testing pregnant sufferers, and others within the state are reportedly contemplating modifications.
As a substitute of automated drug checks, the revised insurance policies use screening questionnaires, which acquire sure info from sufferers, equivalent to their household’s historical past of drug use, and the affected person’s personal historical past and frequency of use. Researchers and main medical teams say these questionnaires are efficient at figuring out somebody with an habit or liable to creating one, which can assist docs steer mother and father into remedy, or decide whether or not a child would possibly want additional medical care. Some hospitals proceed to drug check sufferers below sure circumstances. For instance, at UMass Memorial, pregnant sufferers with recognized substance use issues and new sufferers with none prenatal care are nonetheless drug examined.
The rising motion to restrict drug testing is a supply of optimism for a lot of docs. However its success hinges partly on docs constructing extra significant relationships with their sufferers, so the individuals they deal with really feel inclined to confide about substance use and in the end conform to enter remedy. “That’s actually the aim right here,” stated Dr. Katherine Campbell, chief of obstetrics at Yale New Haven Hospital. “We’re attempting to cut back substance use dysfunction in reproductive-age individuals.”
That will embody asking a affected person for knowledgeable consent to undergo a drug check, and medical personnel being clear about each the aim of the check and its potential authorized penalties.
However some of these conversations could be difficult. Additionally they require longer appointments, one thing many medical establishments are unable or unwilling to offer. “The system is about as much as make it troublesome for us to essentially develop a understanding and trusted relationship with a household,” stated Dr. Lauren Oshman, a household doctor on the College of Michigan Medical College in Ann Arbor.

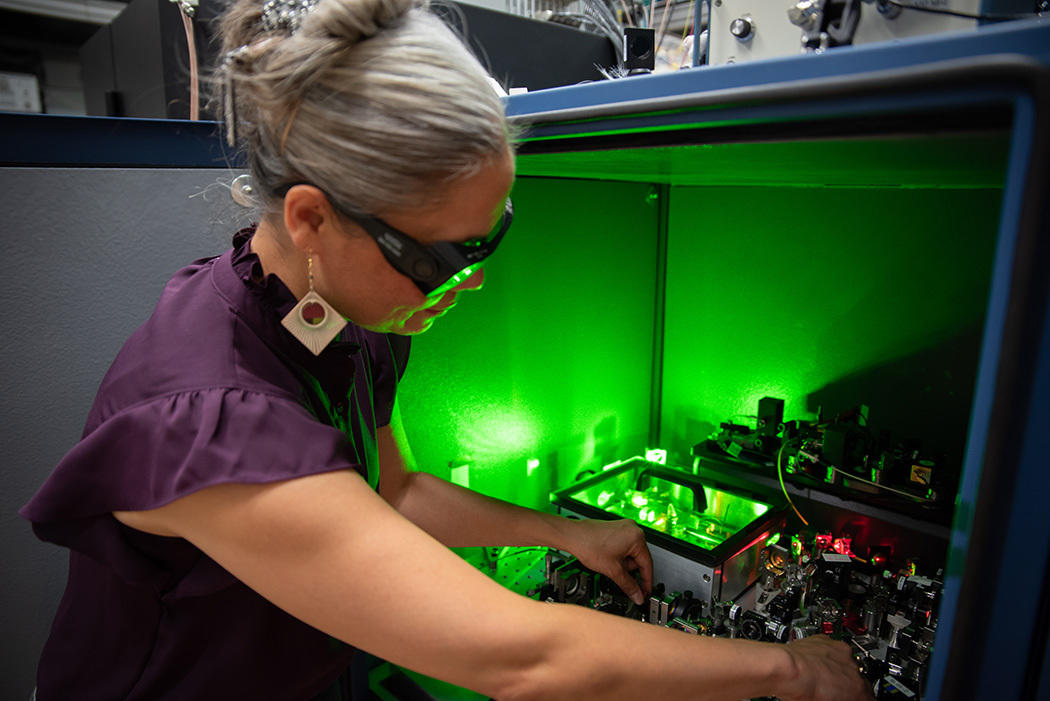
Dr. Lauren Oshman, a household doctor and affiliate professor within the College of Michigan Division of Household Medication, in C.S. Mott Kids’s Hospital in Ann Arbor, Michigan, in February 2025.
By comparability, urine checks are quick and sometimes contain little interplay with sufferers.
“It takes longer to speak to somebody and actually perceive, than it does to position an order and have the individual give a urine pattern,” Campbell stated.
The brand new insurance policies additionally don’t clear up different issues. After Oshman and colleagues found that clinicians at Michigan Medication ordered drug checks for Black newborns extra usually than for White newborns, the hospital community modified its coverage in 2023 to require testing of infants solely in sure circumstances. However early knowledge signifies the brand new coverage had no affect on the racial disparities in testing and reporting.
One purpose, in Oshman’s view, is that Michigan regulation requires the reporting of a affected person whom a supplier “is aware of or suspects” has uncovered their new child to “any quantity” of a managed substance, whether or not authorized or unlawful. That features marijuana, which is authorized in Michigan. When the well being community staff dug into the information, it discovered that for nearly half of all low-risk sufferers whose infants examined constructive, the one drug detected was marijuana, and the sufferers have been most definitely to be Black. Most marijuana-only circumstances don’t lead to findings of abuse or neglect by baby welfare authorities, in accordance with the staff’s analysis. However hospitals are nonetheless required to report these sufferers, Oshman stated.
“And that will not change till the state regulation modifications,” she added.
Hospitals in most different states face comparable challenges. A assessment by The Marshall Challenge discovered that a minimum of 27 states explicitly require hospitals to alert baby welfare companies after a constructive display or potential publicity — although not a single state requires affirmation testing earlier than a report.
Many hospitals which have modified their insurance policies are in states that don’t require reporting constructive checks to baby welfare authorities. In each Colorado and Connecticut, for instance, hospitals are required to report a mother or father provided that suppliers have recognized different security considerations. In Connecticut, suppliers fill out an anonymized kind that permits the state to gather knowledge on substance-exposed newborns with out requiring a baby welfare report.
However even in states that don’t require reporting constructive checks, drug testing stays ubiquitous. For instance, the New York Division of Well being suggested hospitals in 2021 to check labor-and-delivery sufferers solely when “medically indicated” and solely with their consent. However girls proceed to report nonconsensual drug testing at hospitals throughout the state, which has led to them being reported to baby welfare authorities over false constructive and inaccurate outcomes, The Marshall Challenge has discovered.
These challenges present that decreasing the results of drug testing could require a multipronged strategy, from legislative reforms to coverage revisions to enforcement, consultants say.
“We’re simply firstly,” Oshman stated. “That is the beginning of making a system that gives that reliable care.”