April 24, 2025
3 min learn
Key takeaways:
- Ladies with Liletta and Mirena IUDs have been extra more likely to have rosacea 1-year after insertion vs. these with copper units.
- This was not seen with Skyla IUDs, which launch a decrease dose of levonorgestrel.
Hormonal intrauterine units have been related to the next incidence of rosacea in girls in contrast with nonhormonal units, based on a examine.
“We all know that feminine hormones, estrogen and progesterone, each play a job in hormonal pimples, however in addition they play a job within the blushing and flushing mechanisms related to rosacea,” Cameron Rokhsar MD FAAD FAACS, affiliate scientific professor of dermatology at Mount Sinai Hospital, advised Healio. “For instance, when girls are going via menopause, many report blushing, flushing and warmth sensations. That’s all being mediated by fluctuations in estrogen and progesterone.”

Knowledge derived from Arza A, et al. J Am Acad Dermatol. 2025;doi:10.1016/j.jaad.2024.10.029.
Rosacea is a power pores and skin situation characterised by facial erythema and inflammatory pimples lesions. There are numerous environmental components that may set off a rosacea flare, together with excessive warmth or chilly, alcohol consumption, spicy meals and hormonal intrauterine units (IUDs), based on a examine revealed within the Journal of the American Academy of Dermatology.

Cameron Rokhsar
Due to the connections between hormonal fluctuations and blushing, flushing and warmth sensations, authors of this examine analyzed the incidences of rosacea amongst girls with hormonal IUDs in contrast with these with nonhormonal or copper IUDs.
Rosacea charges by IUD sort
Ladies aged 18 to 50 years with a hormonal IUD — Liletta (AbbVie, Medicines360), Mirena (Bayer) or Skyla (Bayer) — have been included within the examine. The researchers evaluated the charges of rosacea incidence 1, 3 and 5 years after IUD insertion. Ladies with rosacea recognized earlier than IUD insertion have been excluded from the examine.
Outcomes confirmed that hormonal IUDs, particularly Liletta and Mirena, have been related to larger charges of rosacea incidence in contrast with copper IUDs.
In contrast with girls who obtained a copper IUD, the incidence charge ratio (IRR) for rosacea 1 12 months after insertion was 1.665 for girls with a Liletta IUD (95% CI, 1.346-0.059). Equally, the IRR for rosacea was 1.389 for girls who obtained a Mirena IUD in contrast with girls who obtained a nonhormonal IUD (95% CI, 0.752-1.533).
This development continued always , based on the researchers. At 3 and 5 years after insertion, the IRR for rosacea was 1.751 (95% CI, 1.481-2.069) and 1.788 (95% CI, 1.530-2.089) for Liletta and 1.44 (95% CI, 1.250-1.656) and 1.472 (95% CI, 1.290-1.678) for Mirena, respectively.
Researchers didn’t observe an associations discovered between Skyla insertion and rosacea incidence, which may very well be because of the slower charge of levonorgestrel, they wrote..
When requested if the IUD was the trigger or just the set off of rosacea amongst these girls, Rokhsar defined that it was almost certainly the set off.
“I don’t consider personally that rosacea is simply brought on by environmental components,” Rokhsar stated. “I consider that you have to have the genetic predisposition for rosacea.”
Remedy choices
Though eradicating the IUD may alleviate the signs, Rokhsar emphasised that dermatologists are properly outfitted to deal with rosacea with out asking sufferers to make such a change.
“We’ve many, many drugs and units at our disposal to get rosacea below management,” Rokhsar stated.
The pimples that accompanies rosacea is greatest handled with oral antibiotics doxycycline, tetracycline and minocycline, in addition to topical antibiotics like metronidazole lotion, clindamycin lotion and ivermectin. Cleansers resembling sodium sulfacetamide can even assist these inflammatory lesions subside.
Blushing and flushing could be partially alleviated via set off avoidance. Based on the Nationwide Rosacea Society, triggers might embrace sure meals, drinks, temperatures, feelings, skincare merchandise and extra.

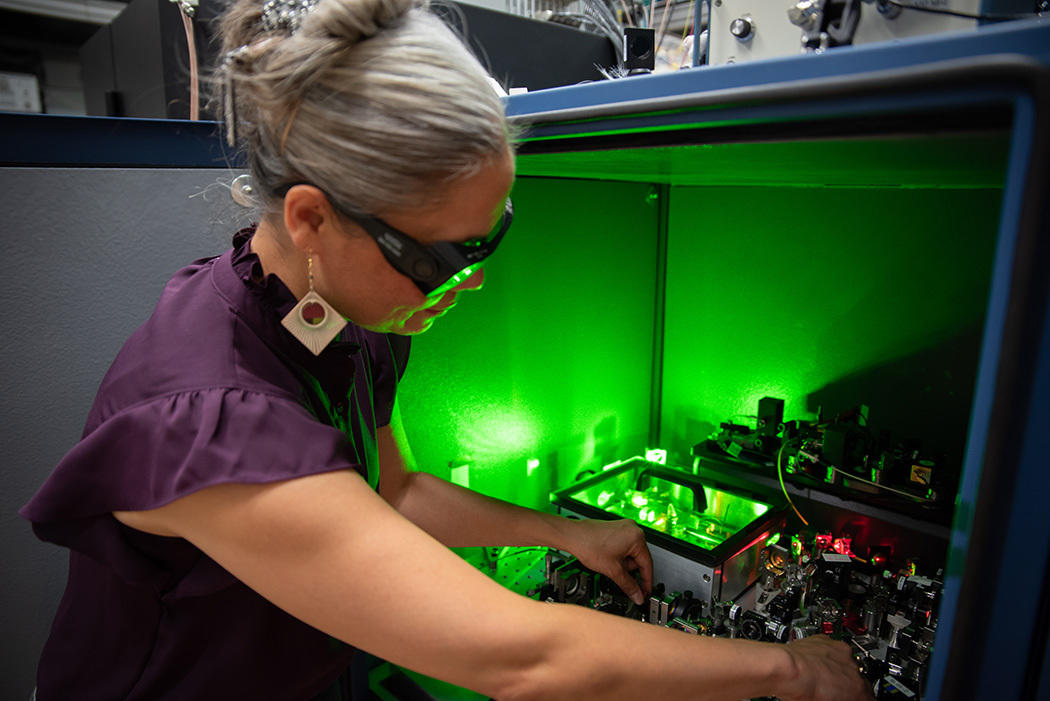
Lycia Thornburg
Lycia Thornburg, MD, FAAD, a dermatologist at Fast Metropolis Medical Middle, advised Healio that environmental triggers are sometimes very particular to the person.
“Sufferers ought to preserve a superb diary of what flares rosacea for them,” Thornburg stated.
Nevertheless, even after the pimples and flushing are addressed, many sufferers usually proceed to expertise telangiectasias. Based on Thornburg, these must be handled with laser remedy.
“For lots of sufferers, telangiectasias trigger them a whole lot of psychosocial misery,” Thornburg stated. “So, the following step is to make use of a laser that has a specific wavelength that treats these blood vessels.”
Thornburg makes use of a 420 nanometer, broadband laser for the primary cross over the pores and skin to deal with the micro organism, adopted by 560 nanometers to focus on the redness of the blood vessels. That is often carried out in a collection of three therapies, Thornburg stated.
Rokhsar agreed, including that dermatologists ought to use pulsed dye laser remedy to manage redness, damaged capillaries and even the general signs related to rosacea, together with pimples.
“At any time when any person says they’ve rosacea, [dermatologists] might preserve throwing antibiotics at sufferers, which doesn’t assist them,” Rokhsar stated. “The antibiotics solely assist the pimples a part of rosacea, however the redness and blushing are in some way intricately related to the event of the pimples half, so it must be emphasised that dermatologists ought to supply the pulsed dye laser.”
For extra data:
Cameron Rokhsar MD FAAD FAACS, could be reached at cameron@put up.harvard.edu.
Lycia Thornburg, MD, FAAD, could be reached at dermatology@healio.com.